Medicare coverage to change on January 30, 2026: and these changes may directly impact how millions of Americans—especially seniors and rural residents—access healthcare via telehealth. Since the COVID-19 pandemic, telehealth has transformed how people “visit” their doctors, but many of the policies that made it possible are now approaching expiration. If you or someone you care for relies on virtual visits with healthcare providers, understanding what’s coming is vital. In this article, we break down what Medicare’s telehealth flexibilities are, what will change in 2026, and how to prepare before those changes take effect.
Medicare coverage to change
January 30, 2026, could mark the end of a groundbreaking era for Medicare telehealth unless lawmakers act quickly. The policies that made virtual care accessible to tens of millions during the pandemic may disappear, reintroducing many of the same geographic, technological, and logistical barriers that telehealth was meant to overcome. While telehealth has proven to be a valuable tool, especially for older adults and underserved populations, the clock is ticking. Whether you’re a patient, a family member, or a healthcare provider, being informed—and taking action—will help you navigate the road ahead. Prepare for a shift that could reshape access to care once again.
| Key Point | Details |
|---|---|
| Policy Change Date | January 30, 2026 – COVID-era Medicare telehealth flexibilities expire |
| What Will Change | Home-based visits, expanded provider list, audio-only coverage, and site/location flexibility may end |
| Who’s Affected | Seniors, people with chronic illness, mental health patients, rural residents |
| Retroactive Coverage | Claims from Oct 1, 2025, to Jan 30, 2026, will be honored under temporary extension |
| Next Steps | Patients and providers should review care plans and prepare for reduced access |
| Official Info | Medicare.gov – Telehealth Coverage |
How Telehealth Changed Healthcare: A Quick Background
Before COVID-19, Medicare only paid for telehealth services in limited situations. Patients had to be in a rural area and physically located at a designated medical facility—not at home—to qualify. This meant people in cities or those too sick to travel were often left out.
When the pandemic hit, everything shifted. In response to the national emergency, Congress and the Centers for Medicare & Medicaid Services (CMS) temporarily lifted restrictions:
- Patients could get care from home.
- All geographic limits were removed.
- More types of providers were eligible to offer services.
- Audio-only calls were covered, allowing access without internet or smartphones.
These flexibilities were extended multiple times and helped millions of Americans stay connected to their care teams.
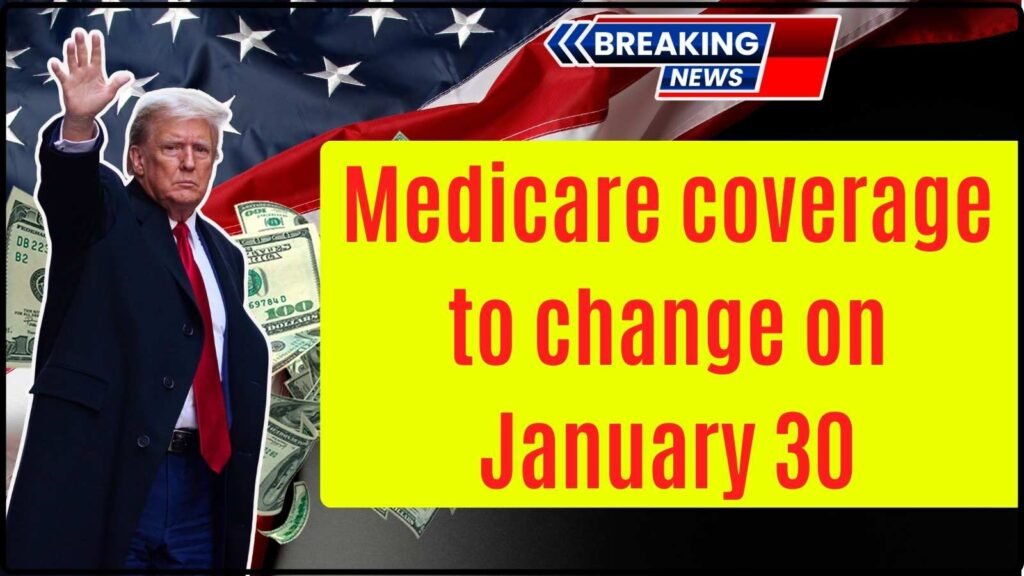
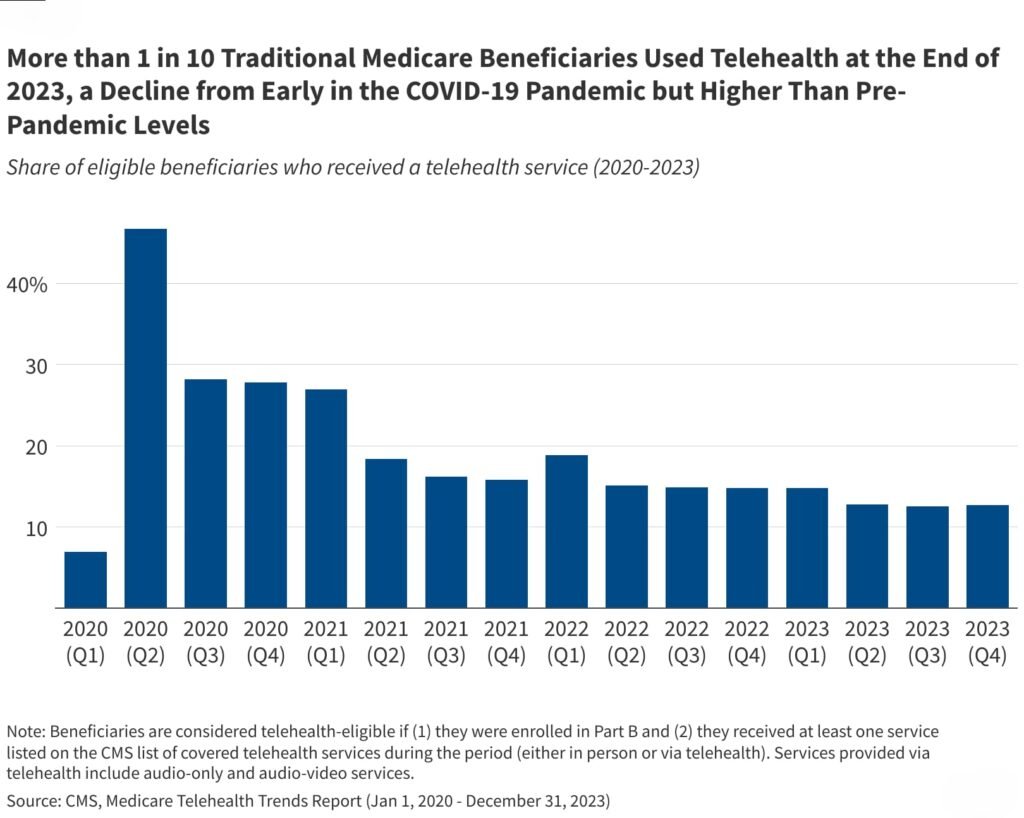
Data Snapshot:
- According to ASPE, 43% of Medicare primary care visits were conducted via telehealth in April 2020.
- A Kaiser Family Foundation (KFF) survey found that 6 in 10 Medicare beneficiaries used telehealth between 2020 and 2022.
- A majority of seniors reported high satisfaction and improved access, especially for behavioral health.
Medicare coverage to change on January 30, 2026?
Unless Congress passes new legislation, most of these flexibilities will expire on January 30, 2026. That means Medicare will revert to pre-pandemic rules for telehealth coverage.
Here’s what that could look like:
1. Location Restrictions Will Return
Under pre-COVID rules, Medicare only covered telehealth if patients were in a rural area and physically present at an approved originating site, such as:
- A doctor’s office
- A hospital
- A rural health clinic
Home-based care will no longer be covered (except in limited cases such as behavioral health).
2. Fewer Providers Will Be Eligible
During the public health emergency, CMS allowed:
- Physical therapists
- Occupational therapists
- Speech-language pathologists
- Audiologists
…to provide services via telehealth. After Jan 30, many of these providers may lose that ability unless a new law passes.
3. Audio-Only Visits May No Longer Count
For seniors without smartphones or Wi-Fi, the ability to call their doctor for a phone-only visit was a huge benefit. This, too, is expected to end, forcing patients to return to video-based or in-person visits.
4. In-Person Visit Requirements Will Return for Mental Health
Medicare waived the requirement for an in-person visit before a tele-mental health visit. After Jan 30, that rule may come back, potentially creating delays or barriers for people seeking psychiatric or counseling services.
Comparison Chart: Then, Now, and 2026
| Feature | Pre-COVID | COVID Era (2020–2026) | Post-Jan 30, 2026 (Expected) |
|---|---|---|---|
| Location Restrictions | Rural area only; must be in clinic | Waived; home allowed | Restrictions return; home excluded |
| Provider Eligibility | Narrow list | Expanded to therapists, FQHCs, etc. | Shrinks unless extended |
| Audio-Only Allowed | No | Yes | Likely no |
| Mental Health via Telehealth | In-person required | In-person waived | Requirement reinstated |
| Patient Access Level | Limited | Broad and inclusive | More limited again |
What Medicare coverage to change Means for You: Practical Steps
Whether you’re a patient, caregiver, or provider, you need to prepare now for what could be a major shift in healthcare delivery.
Patients:
- Talk to your doctor now: Ask if they plan to continue offering telehealth and under what circumstances.
- Prepare for in-person appointments: Especially if you live in an urban area or have mobility challenges.
- Upgrade your tech if possible: While access may shrink, staying video-capable may help bridge the gap.
- Know your rights: If you had a covered telehealth visit between October 1, 2025, and January 30, 2026, and it was denied, you may be eligible for claim reprocessing or reimbursement.
Providers:
- Review Medicare billing practices to avoid penalties.
- Prepare staff and patients for increased in-person demand.
- Stay informed about Congressional updates or potential last-minute extensions.
What the Experts Are Saying?
According to Newsweek, Kevin Thompson, CEO of 9i Capital Group, voiced concern that rural residents and those with disabilities could face major setbacks in care access if the flexibilities are removed.
Physicians across the country, including Dr. Robert Hoyer from Colorado, have publicly warned that ending telehealth access could be a “life or death” issue for some patients, particularly those undergoing cancer treatment or living far from specialists.
These concerns have led to new advocacy efforts to make telehealth permanent under Medicare, with groups pushing for legislation like:
- Telehealth Modernization Act
- CONNECT for Health Act
However, despite bipartisan support, Congress has yet to pass these bills into law.
Patient Story: “Telehealth Saved My Life”
Take the story of Judith, a 76-year-old widow living in rural Arkansas. Before COVID, she had to drive 65 miles to see her endocrinologist. After the pandemic hit, she was able to check in via telehealth every three months—and her diabetes has remained under control.
Now, she’s worried. “If they take it away, I don’t know how I’ll manage. I don’t have anyone to drive me, and I’m not well enough to go on my own.”
Her story reflects the experience of millions of Americans who found that telehealth didn’t just make life easier—it made it possible.
Texas SNAP Payments Set for December 8–14 — Check Payment Dates and Eligibility Criteria
VA Cremation Payouts Revealed: How Much Can Your Family Really Get?
Federal $2,000 Deposit Arriving in December 2025 – Complete Guide for All Beneficiaries